MODE OF ACTION

PREVENTING PRECANCEROUS LESIONS
There is a group of women, who can be labeled as chronic carriers of HPV, in which usual viral clearance does not occur and this is considered high risk for early development of precancerous lesions of the cervix1. This group of HPV-positive women (with the presence of HPV in cervical – or anal – mucus) are not strictly infected. Being infected represents a further step to the viral presence, it means that the HPV has been integrated into the cervical epithelium and has colonized their cells.
Experts speculate four circumstances that may be related to the clearance and persistence of HPV and its ability to colonize the cells of the cervix.
– The viral genotype is the best known variable that determines the capacity of cellular integration and associated oncogenic risk. Genotypes 16 and 18 are critical types2.
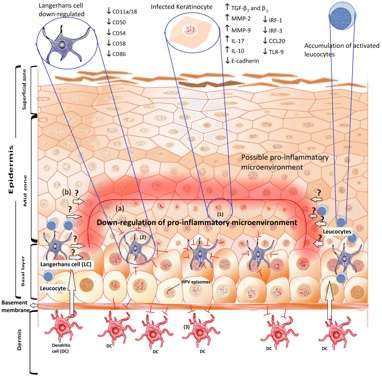
Figure 1. Adapted from A. Amador-Molina Viruses 2013, 5, 2624-2642; doi:10.3390/v5112624. This strategy of HPV is mainly directed to down-regulate the pro-inflammatory response in cervical keratinocytes.
– The immune status of the host is another factor. It is known the high risk of immunocompromised patients for the development of HPV – related lesions3. Recent data has shown a significant correlation between the immune status of women and persistence of high-risk HPV genotypes4. Improving the local immune status, in the area of action of HPV, can be presumed a good strategy to facilitate the clearance of virus.
– The situation of the viral microbiota balance which ensures vaginal health. Recent data clearly demonstrates that this balance determines the pathogenesis of HPV cervical Cancer.
– The histological structure of the ectocervix. HPV needs cells in mitotic activity to integrate6. Cells in the “transformation zone” of the cervix which are in metaplastic re-epithelization process meet this condition, and therefore are ideal targets for anchoring HPV (Figure 3).
Consequently, well epithelized cervix with squamous epithelium, and limited or non-existent transformation areas do not provide a suitable environment for inclusive colonization of HPV.
Therefore, we hypothesize that interfering positively in the three modifiable circumstances outlined above, could be a new preventive strategy of precancerous lesions in HPV-positive women with no strict HPV infection.
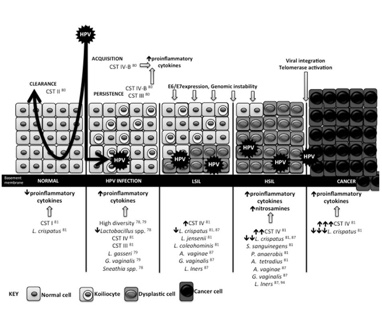
Figure 2. Adapted from Maria Kyrgiou Translational Research DOI: (10.1016/j.trsl.2016.07.004). The vaginal microbiota may play a functional role in the acquisition and persistence of HPV.
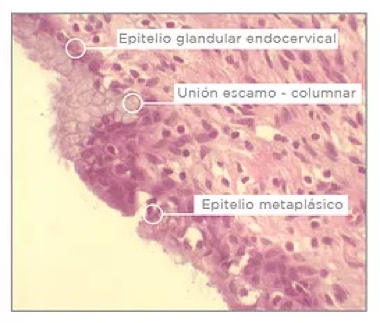
Figure 3. The metaplasic squamous epithelium comes from differentiation and proliferation of reserve cells and is the perfect target for anchoring the HPV.
EFFECT OF A VAGINAL GEL WITH CORIOLUS
VERSICOLOR IN THE EPITHELIZATION
OF THE CERVICAL MUCOSA, VAGINAL MICROBIOTA
AND VAGINAL HEALTH: A PILOT STUDY
The results of a recent research carried out in Spain with a vaginal application gel based on Coriolus versicolor were presented by Dr. Damián Dexeus of the SOMDEX Center-Tres Torres Clinic in Barcelona, in oral communication format, within the session “New insights into molecular biology and markers”.
Papilocare® is a Class IIa medical device in the form of a vaginal gel. This gel has a series of herbal ingredients (hyaluronic acid, Coriolus versicolor, Asian Centella, Azadirachta indica (Neem) and Aloe vera, among others, some of them contained in niosomes and phytosomes, allowing its use as a moisturizing and repairing vaginal mucosa.
The concept of “vaginal health”, such as the state of the vagina that maintains the physiological conditions and a vaginal ecosystem appropriate to the evolution of the age, has gained interest in recent years, also in clinically asymptomatic healthy women. It has been observed that even these women may have alterations of epithelialization of the cervical neck and of the state of the vaginal microbiota.
The objective of this pilot study, presented by Dr Dexeus, was to evaluate the effect of the vaginal application of the Papilocare® gel on epithelization of the cervical mucosa, vaginal microbiota and other vaginal health parameters of asymptomatic women.
An exploratory, open, prospective and non-comparative design included patients between 18 and 45 years of age, without symptoms and vaginal signs and with normal Pap smears, during a routine gynecological control visit. Each patient received instructions for one application of the gel once a day before bed, for 12 consecutive days.
The degree of epithelialization of the cervical mucosa was assessed by colposcopy and was graded by the investigator using a Likert score scale (from 1 = severe ectopia and hemorrhage to 5 = No ectopia). The vaginal microbiota was evaluated using the “Vaginal Status” test developed by the “Institut für Mikroökologie”, Herborn, Germany, and the results of the test were scored by the investigator using a 5-point scale of 1 = very severe deterioration with alteration of all species evaluated at 5 = normal. Bachmann’s Vaginal Health Index (BVV) was also calculated. All evaluations were performed before and 12 days after administration of the vaginal gel.
A total of 21 patients were evaluated (mean age: 32.6 years, range 20-43 years). An improvement in the epithelization of the cervical mucosa was observed: the final mean colposcopy score improved by 43% compared to baseline (3.09 vs 4.42 baseline vs final, Wilcoxon p <0.0001). At the end of the study, 95.3% of the patients improved their degree of epithelialization and a maximum score of 5 was observed in 11 of the 21 women (Figures 2 and 3).
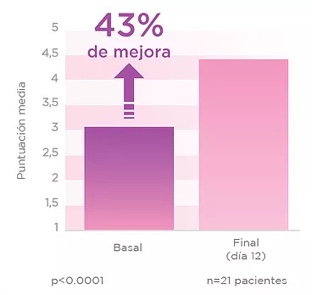
an improvement in the epithelization degree
and 55% got normal
status (score of 5)
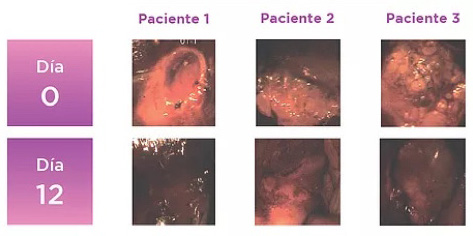
Figure 3. Colposcopic images of 3 patients before and after the application of Palomacare®, in which changes in the epithelization of the cervix are observed.
FALTAM REFERÊNCIAS 5 E 7 NO TEXTO
1. Castellsagué X, Iftner T, Roura E, Vidart JA, Kjaer SK, Bosch FX et al. Prevalence and genotype distribution of human papillomavirus infection of the cervix in Spain: the CLEOPATRE study. J Med Virol. 2012;84:947-56. 2. Moscicki AB, Schiffman M, Burchell A, Albero G, Giuliano AR, Goodman MT et al. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine. 2012; 30Suppl 5:F24-33. 3. Torné A, del Pino M, Cusidó M, Alameda F, Andia D, Castellsagué X et al. Guía de Cribado del Cáncer de Cuello de Útero en España, 2014. Prog Obstet Ginecol 2014; 57(Supl. 1):1-53. 4. Reid JL, Wright TC Jr, Stoler MH, Cuzick J, Castle PE, Dockter J. et al. Human Papillomavirus Oncogenic mRNA Testing for Cervical Cancer Screening: Baseline and Longitudinal Results From the CLEAR Study. Am J Clin Pathol. 2015; 144:473-83. 5. Curso de Colposcopia de la Asociación Española de Patología Cervical y Colposcopia. Disponible en http://www.aepcc.org/ Acceso: 07/09/15. 6. Egawa N, Egawa K, Griffin H and Doorbar J. Human Papillomaviruses: Epithelial Tropisms and the Development of Neoplasia. Viruses. 2015; 7:3863-90. 7. Palacios S.: Pilot study to evaluate the effect of a Coriolus versicolor based vaginal gel on the epithelialization of the cervix lesions. Poster. 30th International Papillomavirus Conference. Septiembre 17-21, 2015. Lisboa. Portugal.